An outbreak of typhoid fever has been reported in El Salvador, with 644 suspected cases from January to the end of May, according to the Minister of Public Health, Violeta Menjívar. The case rate is high across the country, affecting 26 municipalities, including the capital city, San Salvador. Typhoid fever cases increased dramatically this year, compared to the 340 typhoid fever cases reported during the same time period from January to May 2017. El Salvador health authorities have begun monitoring the situation to reduce the spread of disease. [1]
Typhoid fever, more commonly known as typhoid, is a bacterial disease with an estimated 20 million cases and 222,000 fatalities worldwide each year [2]. The causal agent of typhoid is Salmonella Typhi, or Salmonella enterica serotype Typhi, which is a bacterium that breeds in human blood and the intestinal tract. Because severity of illness varies, mild typhoid fever is typically not characterized by its symptoms due to the similarity with other febrile diseases, such as prolonged fever, fatigue, headache, loss of appetite, weakness, abdominal pain, and constipation or diarrhea. Therefore, a blood test is the only reliable way to diagnosis typhoid fever by identifying the presence of Salmonella Typhi.
Salmonella Typhi lives only in humans [3]. The bacteria can be transmitted from both active patients and recovered patients. Although symptoms disappear, the agent is still carried by those that have recovered, and can contaminate food and water through feces [4]. Poor sanitation, handling food without washing hands, and lack of clean drinking water, all significantly contribute to typhoid fever outbreaks among poor communities, where children are one of the most vulnerable populations.
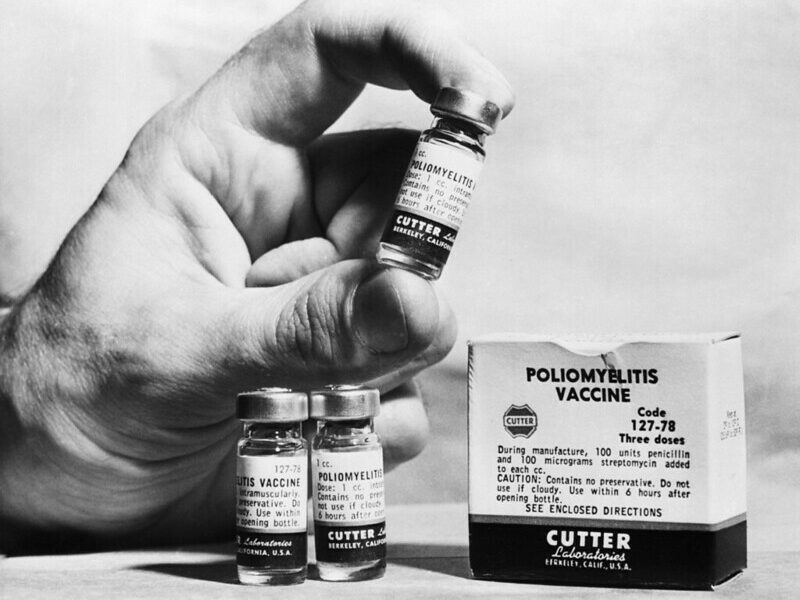
Fortunately, typhoid fever is preventable and treatable. People can reduce their risk of exposure by washing hands, consuming thoroughly-cooked food and drinking boiled water in the areas with high prevalence of disease. Additionally, vaccination is also available for prevention; however, it is not 100% effective and cannot provide lifelong immunity [2]. According to World Health Organization (WHO), the single-shot injectable Vi capsular polysaccharide vaccine (ViCPS) has estimated 72% protective efficacy in the first 1.5 years in the high-risk areas, and revaccination is recommended every three years [5]. For the oral Ty21a vaccine, revaccination is recommended every five years by US Center for Disease Control and Prevention (CDC) [6]. For local health authorities, providing adequate sanitation, offering health education and improving the public health surveillance system are compelling and necessary strategies to control the typhoid fever epidemic.
Typhoid fever is often treated with antibiotics and supportive care. Antibiotics, such as ampicillin, chloramphenicol, trimethoprim/sulfamethoxazole, amoxicillin, and ciprofloxacin, have historically been used for typhoid fever treatment. With supportive care, the proper antimicrobial therapy decreases mortality rates to around 1% [7]. However, as antibiotic resistance becomes a growing global issue, most medicines mentioned above are no longer used as first-line treatment for typhoid [8]. Instead, ceftriaxone or azithromycin are recommended for people who are infected with multidrug-resistant typhoid [9]. With limited antibiotic options available, and high selective pressure on S. Typhi, experts are concerned that one more genetic mutation may create an antibiotic resistant typhoid fever which will be untreatable in areas like Southeast Asia and parts of Africa [10].
Sources:
[1] http://outbreaknewstoday.com/el-salvador-reports-increase-in-typhoid-fever-21047/
[2] http://www.who.int/immunization/diseases/typhoid/en/
[3] http://www.who.int/mediacentre/factsheets/typhoid/en/
[4] https://www.cdc.gov/typhoid-fever/symptoms.html
[5] http://www.who.int/ith/vaccines/typhoidfever/en/
[6] https://www.cdc.gov/typhoid-fever/typhoid-vaccination.html
[7] https://web.archive.org/web/20111102190825/http://www.who.int/vaccine_research/diseases/diarrhoeal/en/index7.html
[8] http://mbio.asm.org/content/9/1/e00105-18.full
[9]http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004530.pub4/abstract;jsessionid=F84E63F93C0BB05EA48F6DAB8D2372AA.f01t02
[10] https://www.nytimes.com/2018/04/13/health/drug-resistant-typhoid-epidemic.html